- endometrium up to 6 mm
1. CAUSES
Thin endometrium can be caused by various factors, including:
HORMONAL DISORDERS: A lack of progesterone, excess estrogen, or dysfunction of the pituitary or thyroid glands can lead to improper endometrial growth.
Thin endometrium can be caused by various factors, including:
HORMONAL DISORDERS: A lack of progesterone, excess estrogen, or dysfunction of the pituitary or thyroid glands can lead to improper endometrial growth.
MENSTRUAL CYCLE DISORDERS: Amenorrhea, oligomenorrhea, and other cycle disorders can result in insufficient endometrial development.
REPRODUCTIVE SYSTEM DISEASES: Polycystic ovary syndrome (PCOS), endometriosis, uterine fibroids, and infectious diseases of the reproductive organs can affect endometrial thickness.
CHRONIC STRESS: Stress can disrupt hormonal balance, affecting hormone production and the condition of the endometrium.
MEDICATIONS: The use of certain medications, such as hormonal drugs, contraceptives, and chemotherapy drugs, can negatively impact the endometrium.
SURGICAL INTERVENTIONS: Including abortions, curettage, and uterine surgeries, which can damage the endometrium. This also includes
* ASHERMAN'S SYNDROME
This condition is characterized by the formation of adhesions in the uterine cavity, which can lead to impaired normal uterine and reproductive system function. Adhesions often occur after traumatic interventions in the uterine cavity, such as curettage (including after abortion, miscarriage, or diagnostic curettage), cesarean section, or infectious diseases.
Main characteristics of Asherman's syndrome:
Adhesion formation: Tissues inside the uterus fuse, which can lead to partial or complete uterine obstruction.
Main symptoms:
Absence or significant reduction of menstruation (amenorrhea or hypomenorrhea).
Painful menstruation.
Infertility or difficulty conceiving.
Sometimes, lower abdominal pain and discomfort during intercourse may occur.
Causes of Asherman's syndrome:
Postoperative complications: uterine curettage after abortion, miscarriage, surgeries, or diagnostic procedures.
Infectious diseases: Inflammations, such as endometritis, can lead to adhesion formation.
Circulatory problems in the uterus after surgeries or injuries.
DIAGNOSIS:
Ultrasound (US) — helps identify changes in the uterine cavity.
Hysteroscopy — the main diagnostic method, where a special device (hysteroscope) is used to examine the uterine cavity and remove adhesions if present.
Hysterosalpingography (HSG) — an X-ray examination with contrast material to visualize adhesions.
TREATMENT:
Surgical intervention (hysteroscopy) to remove adhesions and restore the normal uterine cavity.
In some cases, hormonal therapy (e. g. , estrogens) may be required to improve the endometrium's condition post-surgery and prevent reformation of adhesions.
AGE: In women over 40, age-related changes in the reproductive system can lead to reduced endometrial thickness.
CIRCULATION PROBLEMS: Poor blood supply to the uterus can hinder normal endometrial growth.
RECENT PREGNANCY: After miscarriage or childbirth, endometrial recovery may take time, especially if complications occurred.
2. SYMPTOMS
Scanty or irregular menstruation.
Lower abdominal pain before or after menstruation.
Miscarriages or unsuccessful IVF attempts.
3. DIAGNOSIS
Pelvic ultrasound: Assessment of endometrial thickness and structure in different phases of the menstrual cycle: days 8–10 and 19–21 of the cycle.
In unsuccessful IVF attempts, tests such as. . .
E. R. A. (endometrial receptivity analysis) using NGS
- used to determine endometrial readiness for implantation. Pre-receptive, receptive, post-receptive endometrium – conducted after 5 days of progesterone intake or in a natural cycle.
EMMA (endometrial microbiome metagenomic analysis) – assessment of endometrial microbiota composition. Lactobacilli dominate.
ALICE (analysis of infectious chronic endometritis) – detection of endometritis signs. Chronic endometritis may not cause any symptoms.
CD-138 determination for endometritis signs.
Dopplerometry: study of blood flow in uterine vessels.
Hysteroscopy: examination of the uterine cavity to identify adhesions or other pathologies.
Endometrial biopsy – PIPE biopsy
4. TREATMENT. PREPARATION for IVF
Estrogens
Tablets, transdermal forms, injections to stimulate endometrial growth – Ethinyl Estradiol (Progynova, Estrogel, Divigel. . ), Estrogen patches (EVRA, Dermestril 25mg, 50mg)
Progesterone: helps prepare the endometrium for implantation – Utrogestan, Ingesta, Duphaston.
FEMOSTON
Normal blood supply promotes endometrial growth. For this, the following are used:
Vascular drugs – Phlebodia, Detralex…
B vitamins (B6, B9, B12), E, C – "Milan cocktail" IV course 5-7 days, Mionevrazi IM
Normast mps 300/600mg to stimulate receptors
Folic acid Italy on a regular basis. .
Vitamin D – Dibaza 300,000 IU (with subsequent vitamin D level control)
Enzyme preparations.
Nitric oxide donor groups.
Human IMMUNOGLOBULIN - Bioven
PRP — autologous blood plasma enriched with platelets 4–5 times above normal. It stimulates proliferation and regeneration through numerous growth factors. PRP can promote endometrial growth, thickness, and structural changes. It can be used to irrigate the uterus or inject into the endometrial walls under visual control.
EXOSOMES for endometrial growth stimulation?
Physiotherapy
Diet
Foods rich in vitamin E: nuts, seeds, olive oil, avocado.
Iron-rich foods: red meat, liver, beets, spinach.
Foods with omega-3 fatty acids: fish (salmon, sardines), flaxseed.
Antioxidants: berries, green tea, broccoli.
STRESS
Massage; sleep at least 7–8 hours a day; activity throughout the day, magnesium supplements (Italy)
SURGICAL treatment
Hysteroscopy, Hystero-resectoscopy
#######
DR. RECKEWEG PREPARATIONS FOR THE ENDOMETRIUM!
Dr. Reckeweg offers several preparations that can be used to support endometrial health in women. They help improve blood supply, hormonal balance, and restore reproductive system functions. Let's consider the most suitable:
Preparations for the endometrium:
1. R20 – For hormonal balance disorders
Purpose: Regulates ovarian function, supports estrogen and progesterone balance.
Indications:
Endometrial hypoplasia (thin endometrium).
Menstrual cycle disorders.
Luteal phase deficiency.
Dosage:
1 tablet or 10 drops 3 times a day.
2. R1 – Anti-inflammatory preparation
Purpose: Relieves inflammatory processes in the pelvic organs.
Indications:
Endometritis.
Chronic inflammatory endometrial diseases.
Dosage:
In acute conditions: 1 tablet or 10 drops every 1–2 hours.
In chronic conditions: 1 tablet or 10 drops 3 times a day.
3. R10 – For the female reproductive system
Purpose: Improves blood supply to pelvic organs, regulates the cycle.
Indications:
Endometrial hypoplasia.
Dysmenorrhea, irregular or painful menstruation.
Dosage:
1 tablet or 10 drops 3 times a day.
4. R2 – To improve circulation
Purpose: Improves microcirculation and tissue nutrition, including the endometrium.
Indications:
Weak blood flow in pelvic organs.
Dosage:
1 tablet or 10 drops 3 times a day.
Recommendations for endometrial support:
Comprehensive approach:
For endometrial hypoplasia: combine R20 and R10.
For inflammation: supplement treatment with R1.
For poor circulation: include R2.
Course duration:
At least 2–3 months, depending on the condition.
Sample regimen:
Morning: R20 + R10 (1 tablet or 10 drops each).
Day: R10 + R2 (1 tablet or 10 drops each).
Evening: R20 + R1 (1 tablet or 10 drops each)
36у.е.
1 vial of lyophilized powder contains: Cyanocobalamin (Vitamin B12) 1 mg, Pyridoxine hydrochloride (Vita...
Докладніше 150у.е.
Scientific names: Cordyceps Militaris, Cordyceps Sinensis Wild Cordyceps Sinensis – Caterpillar Fungus
Докладніше 34у.е.
Active ingredients: Each patch with an area of 20 cm² contains 6.0 mg of norelgestromin and 0.60 mg of ethinyl...
Докладніше 178у.е.
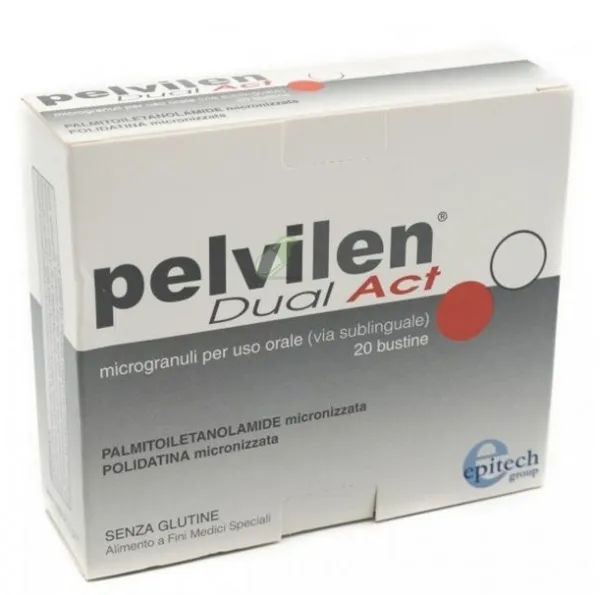
Active ingredients: ultra-micronized palmitoylethanolamide, micronized palmitoylethanolamide.
ДокладнішеActive ingredient: Human normal immunoglobulin for intravenous administration; 1 ml of the preparation conta...
ДокладнішеComposition: Apis mellifica D6, Belladonna D6, Calcium iodatum D12, Kalium bichromicum D12, Marum verum D6,...
ДокладнішеComposition: • Acidum sulfuricum D4 (Sulfuric acid D4) • Cimicifuga D4 (Cimicifuga D4) • Lachesis D12 (Lachesi...
ДокладнішеComposition (per 1 g): • Sus scrofa D12 (Adrenal glands) • Sus scrofa D12 (Ovaries) • Sus scrofa D12 (Pancreas...
ДокладнішеActive Ingredients Daily Dose (2 tablets) • Revifast® with trans-resveratrol 160 mg, 48 mg. • Trans-resverat...
Докладніше 65у.е.
Composition: Ultramicronized Palmitoylethanolamide — 200 mg, Palmitoylethanolamide in co-micronized form wit...
Докладніше