We offer both classical and experimental approaches for the treatment or correction of this condition, as well as treatment by 36‐hour fasting and therapy with the NEEL medication.
We offer both classical and experimental approaches for the treatment or correction of this condition, as well as treatment by 36‐hour fasting and therapy with the NEEL medication. . .
1. CLASSICAL RECOMMENDATIONS:
Insulin resistance is a condition in which the body's cells lose sensitivity to insulin, leading to an increase in blood glucose and insulin levels. Effective treatment includes a combination of lifestyle changes, medication therapy, and, if necessary, additional methods.
1. Lifestyle Changes
Diet:
• Reduce consumption of simple (fast) carbohydrates:
Eliminate sugar, sweets, white bread, mashed potatoes, and white rice.
• Prefer complex carbohydrates:
Whole grain products, quinoa, oats.
• Increase fiber intake:
Vegetables, fruits with a low glycemic index (berries, apples);
Flax seeds, chia seeds, bran.
• Balance your diet:
Include protein in every meal (fish, chicken, eggs, legumes).
• Include healthy fats:
Avocado, nuts, olive oil.
• Limit saturated fats:
Avoid trans fats (fast food, pastries) and fatty meats.
Physical Activity
• Strength training:
Improves muscle sensitivity to insulin.
Recommended 2–3 times per week.
• Aerobic activity:
Walking, running, swimming — 30–60 minutes a day.
Supports overall metabolism.
• Active lifestyle:
Minimize prolonged sitting; add movement throughout the day.
Weight Control
• Losing 5–10% of body weight significantly improves insulin sensitivity.
• Maintain a caloric deficit through proper diet and physical activity.
2. Medication Therapy
• Metformin:
First-line medication.
Reduces glucose production in the liver and improves tissue sensitivity to insulin.
Recommended dosage: from 500 mg to 2000 mg per day (as prescribed by a doctor).
• SGLT-2 Inhibitors:
Help remove excess glucose via the kidneys.
Examples: dapagliflozin, empagliflozin.
• GLP-1 Agonists:
Reduce appetite and stimulate insulin secretion.
Examples: semaglutide (Ozempic), liraglutide (Saxenda).
• Thiazolidinediones (glitazones):
Increase insulin sensitivity.
Example: pioglitazone.
• Additional Medications:
Alpha-lipoic acid: an antioxidant that increases insulin sensitivity.
Omega-3 fatty acids: reduce inflammation associated with insulin resistance.
3. Additional Measures
• Stress Management
Chronic stress raises cortisol levels, which worsens insulin resistance.
Practice meditation, yoga, or deep-breathing techniques.
• Sleep Quality
Sleep deprivation worsens insulin sensitivity.
Aim for 7–9 hours of quality sleep per day.
• Regular Medical Monitoring
Monitor blood glucose, insulin, and HbA1c (glycated hemoglobin).
Check lipid profile and markers of inflammation.
4. Natural Supplements and Nutraceuticals
• Berberine:
A natural remedy with a mechanism of action similar to metformin.
Dosage: 500 mg 2–3 times per day.
• Magnesium:
Involved in regulating blood sugar levels.
Sources: nuts, leafy greens, mineral supplements.
• Chromium:
Helps improve carbohydrate metabolism.
• Vitamin D:
Deficiency is associated with worsened insulin sensitivity.
Recommended to take based on lab tests.
––––––––––––––––––––––––––––––––––––––––––––––––––
2. EXPERIMENTAL METHODS FOR CORRECTING INSULIN RESISTANCE
. . . These are in the stage of clinical or laboratory research and are aimed at a deeper understanding of the disease mechanisms. The main directions of these methods include:
1. Hormone and Peptide Therapy
• Next-generation GLP-1 Agonists
– Medications such as semaglutide and tirzepatide have dual actions: they increase tissue sensitivity to insulin and regulate appetite.
– Tirzepatide (Mounjaro) combines the activity of GLP-1 and GIP, improving glucose metabolism and promoting weight loss.
• GDF15 (Growth Differentiation Factor 15)
– A protein associated with appetite control that contributes to weight loss and improved insulin sensitivity.
• FGF21 (Fibroblast Growth Factor 21)
– A hormone involved in regulating energy metabolism; it activates lipolysis processes and improves tissue insulin sensitivity.
2. Genetic Therapy
• CRISPR/Cas9 for Gene Modification
– Used to correct genes related to insulin metabolism. For example, researchers are exploring modification of the IRS1 gene, which is involved in insulin signal transduction.
• MicroRNA (miRNA) Therapy
– Specific microRNAs regulate the expression of genes responsible for insulin sensitivity. For instance, suppressing miR-29 may improve insulin sensitivity.
3. Cell and Tissue Transplantation
• Pancreatic Beta-cell Transplantation
– Beta-cells can be transplanted to restore normal insulin secretion.
• Stem Cell Therapy
– The use of mesenchymal stem cells to reduce inflammation and restore metabolic functions.
• Microbiota
– Fecal Microbiota Transplantation (FMT) to restore the balance of intestinal bacteria, which may improve glucose metabolism.
4. Technologies and Devices
• Implantable Devices for Insulin and Hormone Delivery
– Bionic systems for automatically regulating insulin and other metabolic hormones.
• Vagal Nerve Electrical Stimulation
– A method aimed at improving metabolism by activating neural pathways related to glucose regulation.
5. Experimental Dietary Approaches
• Ketogenic Diets and Nutritional Modulation
– The use of low-carbohydrate, high-fat diets to alter metabolism and increase tissue insulin sensitivity.
• Dietary Supplements
– Research is exploring the effects of curcumin, resveratrol, polyphenols, and alpha-lipoic acid for reducing inflammation and improving glucose uptake.
6. Mitochondrial Function-Based Therapy
• Targeted Mitochondrial Activation
– Medications aimed at improving mitochondrial function, such as MitoQ and SS-31, which help increase energy metabolism.
• NAD+ (Nicotinamide Adenine Dinucleotide)
– Increasing NAD+ levels through precursors like NR (nicotinamide riboside) improves metabolism and restores cellular function.
7. Experimental Methods of Neuroregulation
• Transcranial Magnetic Stimulation (TMS)
– A technique that acts on the brain to improve the regulation of appetite and metabolism.
• Deep Brain Stimulation (DBS)
– Being studied as a method to correct hypothalamic disturbances that affect glucose metabolism.
8. New Medicinal Drugs
1. Cytokine Inhibitors:
• Cytokines such as TNF-α are involved in the inflammation associated with insulin resistance.
2. Inhibitors of Inflammatory Cascades:
• Medications that reduce tissue inflammation (for example, NLRP3 inflammasome inhibitors).
3. Selective PPAR-γ Receptor Activators:
• For example, improved formulations of pioglitazone designed to minimize side effects.
9. MOTS-c – This is a mitochondria-derived peptide with promising properties in regulating metabolism and preventing metabolic diseases. The main aspects are:
1. Mechanism of Action
• Affects mitochondrial function and modulates oxidative metabolism processes.
• Regulates insulin sensitivity, carbohydrate metabolism, and energy expenditure.
2. Clinical Effect
• Being studied for the treatment of obesity, insulin resistance, and age-related metabolic changes.
• Reduces fat mass, improves glucose metabolism.
3. Formulation
• In this case, it is presented as a ready-to-use pre-filled pen (Pre-filled pen GoQuick).
4. Application
• Subcutaneous injections, 10 mg/2 ml.
5. Perspectives
• May be used in combination with other therapeutic agents for treating type 2 diabetes, obesity, and metabolic syndrome.
––––––––––––––––––––––––––––––––––––––––––––––––––
3. 36-HOUR FASTING TREATMENT
A 36-hour fast is one form of intermittent fasting, which is increasingly being considered as an effective approach for improving insulin sensitivity and glucose metabolism. This method has several physiological effects that can be beneficial in insulin resistance. Here is detailed information:
Mechanisms of 36-Hour Fasting
• Reduction in Insulin Levels
During fasting, insulin levels drop, allowing the body's cells to "rest" from constant exposure to the hormone. This improves tissue sensitivity to insulin.
• Increased Lipolysis and Ketogenesis
After 12–16 hours without food, the body begins to use fat as its primary energy source. This contributes to a reduction in visceral fat, which is linked to insulin resistance.
• Improvement in Mitochondrial Function
Fasting stimulates autophagy – the process of cleaning out damaged mitochondria and proteins, which enhances cellular function.
• Reduction in Inflammation
A 36-hour fast helps decrease the chronic inflammation that is one of the factors in insulin resistance.
• Stimulation of Receptor Sensitivity
Increased activity of GLUT-4 receptors, which are responsible for transporting glucose into muscle cells.
• Normalization of Blood Sugar Levels
Intermittent fasting helps stabilize blood glucose, preventing sudden spikes and drops.
Advantages of 36-Hour Fasting for Insulin Resistance
• Rapid decrease in blood glucose and insulin levels.
• Reduction of body weight and visceral fat.
• Improvement in the lipid profile (lowering triglycerides and “bad” cholesterol).
• Increased secretion of metabolism-regulating hormones (e. g. , adiponectin).
• Potential reduction in the risk of developing type 2 diabetes.
How to Practice 36-Hour Fasting (Author’s Method):
• Begin on Friday after dinner, typically around 9:00 PM.
• Finish on Sunday at 9–10:00 AM after doing some exercise outdoors.
• The most critical period occurs at night.
Thus – you must fast for 2 nights! ! !
Method:
– Drink water freely whenever you feel like it (preferably warm, not mineral water—clean water is best; if available, artesian water, or any other clean water).
Breaking the fast – start with grapefruit, kefir, tsorog (a type of cultured dairy product), berries, apples, avocado (until 3:00 PM), then resume normal eating.
Risks and Limitations:
• Hypoglycemia
In patients with pronounced insulin resistance and impaired blood sugar regulation, glucose levels may drop too low.
• Chronic Stress on the Body
If 36-hour fasts are performed too frequently, they can trigger a stress response and raise cortisol levels, which negatively affects insulin sensitivity.
Contraindications:
• Pregnancy, lactation.
• Underweight individuals, eating disorders.
• Serious liver or kidney diseases.
• Adaptation of the Body
Transitioning to fasting may cause dizziness, weakness, or irritability.
Scientific Data:
Research shows that intermittent fasting, including 36-hour cycles, can:
• Reduce fasting glucose and insulin levels by 20–30%.
• Increase tissue insulin sensitivity (as per HOMA-IR data).
• Contribute to a 3–5% reduction in fat mass over several months.
Practical Recommendations:
• Start with shorter fasting periods (12–16 hours) so the body can adapt.
• Maintain normal water-electrolyte balance (use mineral water and add a little salt to it).
• Monitor how you feel: if you experience severe weakness or dizziness, stop fasting.
• Consult a doctor before starting, especially if you take medications to lower blood sugar (e. g. , metformin).
A 36-hour fast can be a powerful tool in combating insulin resistance when applied correctly. However, it should be part of an overall plan that includes physical activity, balanced nutrition, and medication therapy (if necessary).
––––––––––––––––––––––––––––––––––––––––––––––––––
NB!
FORMS OF TYPE 2 DIABETES NOT RELATED TO INSULIN RESISTANCE:
Type 2 diabetes is most often associated with insulin resistance (for example, type 2 diabetes), but there are forms whose development is driven by other pathophysiological processes. These forms include autoimmune, genetic, endocrine, and iatrogenic causes.
1. Latent Autoimmune Diabetes in Adults (LADA)
Description:
LADA is a slowly progressing form of autoimmune diabetes. It develops in adults over 30, but outwardly it may resemble type 2 diabetes.
Mechanism:
Autoimmune destruction of pancreatic beta-cells leads to reduced insulin secretion. In the early stages, insulin sensitivity is usually normal.
Characteristics:
Slow progression.
Presence of antibodies to GAD, IA-2, or other antigens.
Eventually requires insulin therapy.
2. Genetic Forms of Diabetes (e. g. , MODY)
Description:
MODY (Maturity-Onset Diabetes of the Young) comprises monogenic forms of diabetes caused by mutations in genes that regulate beta-cell function.
Mechanism:
Impaired insulin secretion with preserved tissue sensitivity to insulin.
Examples:
• MODY2: A mutation in the glucokinase gene, which alters the glucose-sensing threshold.
• MODY3: Mutation in HNF1A, which reduces insulin secretion.
Characteristics:
Diagnosed at a young age.
Treatment may include diet, oral medications, or insulin depending on the MODY type.
3. Pancreatic Damage
Description:
Diabetes develops as a result of the loss of functional pancreatic tissue.
Mechanism:
A reduced number of beta-cells leads to decreased insulin secretion.
Causes:
• Chronic pancreatitis.
• Surgical removal of part of the pancreas.
• Cancer or other pancreatic diseases.
Characteristics:
Often accompanied by impaired secretion of other pancreatic hormones (glucagon, somatostatin).
4. Endocrine Diseases
Description:
Diseases associated with excessive hormone secretion that interferes with insulin action.
Examples:
• Cushing’s syndrome: Excess cortisol reduces tissue sensitivity to insulin.
• Acromegaly: Excess growth hormone impairs insulin action and enhances glycogenolysis.
• Pheochromocytoma: Catecholamines stimulate glycogenolysis and inhibit insulin.
Characteristics:
Primary treatment focuses on correcting the underlying disease.
5. Diabetes Caused by Medications or Toxins
Description:
Certain medications and toxins can damage beta-cells or impair their function.
Examples:
• Glucocorticoids.
• Immunosuppressants (e. g. , calcineurin inhibitors).
• Thiazide diuretics.
• Alcohol and toxic substances.
Mechanism:
Reduced insulin secretion without pronounced insulin resistance.
6. Gestational Diabetes with Progression
Description:
In some women, gestational diabetes progresses to permanent diabetes due to impaired insulin secretion.
Characteristics:
Insulin sensitivity remains normal, but the beta-cells’ compensatory secretion ability is diminished.
7. Post-Transplant Diabetes
Description:
Diabetes that develops after organ transplantation due to the effects of immunosuppressants (calcineurin inhibitors, corticosteroids).
Mechanism:
Medications damage beta-cells or suppress their function.
Conclusion:
The forms of diabetes not associated with insulin resistance are diverse in their mechanisms and causes. Their common feature is impaired insulin secretion with preserved or only partially altered tissue sensitivity to insulin. Diagnosing and treating these forms requires an individualized approach, including genetic tests, antibody analysis, functional diagnostics of the pancreas, and therapy aimed at eliminating the underlying cause.
––––––––––––––––––––––––––––––––––––––––––––––––––
Treatment of Insulin Resistance with German Homeopathic Medications Dr. Reckeweg:
For targeted treatment of insulin resistance, the most suitable Dr. Reckeweg medications are R40 and R59, as well as their combination.
Main medication – R40!
✓ Objective: Improves carbohydrate metabolism, regulates pancreatic function, reduces blood sugar levels, and lowers insulin resistance.
✓ Effects:
• Enhances the cells’ sensitivity to insulin.
• Regulates carbohydrate metabolism and prevents blood sugar fluctuations.
• Improves the function of the liver, pancreas, and blood vessels.
✓ Dosage:
10 drops 3 times a day before meals, or dissolve 1 tablet 3 times a day.
Course: 3 months, followed by monitoring of insulin and glucose levels.
Additional medication – R59 (for metabolic syndrome and obesity)!
✓ Objective: Improves fat metabolism, reduces visceral fat (which provokes insulin resistance).
✓ Effects:
• Reduces insulin resistance by decreasing obesity.
• Accelerates metabolism and supports the liver in processing fats.
✓ Dosage:
10 drops 3 times a day or 1 tablet 3 times a day.
Course: 2–3 months, followed by a repeat analysis.
How to combine them?
Medication Scheme for Treating Insulin Resistance:
• Morning: R40 + R59 (10 drops or 1 tablet each).
• Day: R40 (10 drops or 1 tablet).
• Evening: R40 + R59 (10 drops or 1 tablet each).
⏳ Course: 3 months, then a blood test for HOMA-IR (insulin resistance index).
Additional Recommendations:
✓ Dietary correction: Reduce simple carbohydrates and increase protein intake.
✓ Physical activity: Moderate exercise 3–4 times per week improves insulin sensitivity.
✓ Control metabolic parameters: Glucose, insulin, HOMA-IR.
––––––––––––––––––––––––––––––––––––––––––––––––––
Conclusion
Non-metformin strategies for treating insulin resistance encompass a wide range of mechanisms—from the activation of nuclear receptors to the modulation of gut hormones and inflammation. Thiazolidinediones reprogram adipocyte metabolism, reducing lipotoxicity and inflammation, thereby restoring the sensitivity of insulin receptors in muscles and the liver. GLP-1 agonists and SGLT-2 inhibitors reduce glycemia and body weight through various pathways, resulting in improved insulin signaling and decreased hyperinsulinemia. Antioxidants and anti-inflammatory agents target the pathogenetic factors of insulin resistance—oxidative stress and chronic inflammation—and may serve as adjuncts to enhance the overall effect. New developments, such as multivalent hormone agonists (for example, tirzepatide) or inhibitors of negative regulators of the insulin pathway (PTP1B inhibitors, blockers of inflammatory cascades), show promising results in restoring insulin receptor sensitivity.
An optimal approach will likely include a combination of several medications that address different levels: improving insulin signaling within the cell, reducing stress factors (hyperglycemia, lipotoxicity), reducing weight, and suppressing chronic inflammation.
Individualized therapy, which takes into account comorbid conditions (such as hypertension, dyslipidemia, fatty liver disease), will maximize the synergistic effects of the medications. With ongoing clinical research and the advent of new agents, the prospect of effectively “reprogramming” insulin-resistant receptors without metformin is becoming increasingly realistic, offering hope for improved outcomes in patients with metabolic disorders.
150у.е.
Scientific names: Cordyceps Militaris, Cordyceps Sinensis Wild Cordyceps Sinensis – Caterpillar Fungus
Докладніше 38у.е.
4 capsules contain: Coriander, lyophilized fruit extract - 350 mg, standardized to 2% phenols - 7 mg Ginger...
Докладніше 33у.е.
Composition Acidum phosphoricum D12, Arsenicum album D8, Lycopodium D30, Natrium sulfuricum D12, Secale corn...
Докладніше 63у.е.
Average content of active ingredients (per 2 tablets): • α-lipoic acid – 800 mg • PEA (palmitoylethanolamide...
Докладніше 178у.е.
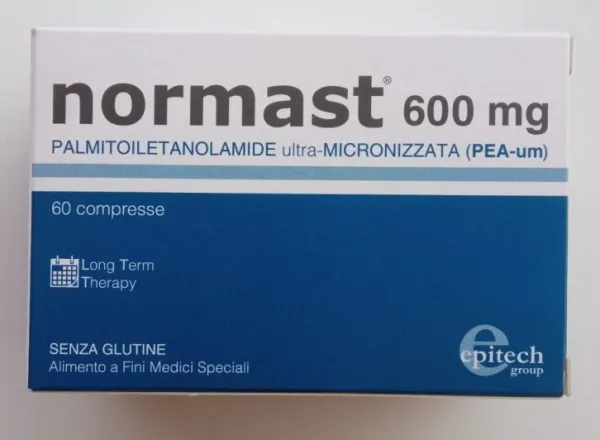
Active ingredients: ultra-micronized palmitoylethanolamide, micronized palmitoylethanolamide.
Докладніше 100у.е.
COMPOSITION: Ultramicronized palmitoylethanolamide 600 mg; excipients: microcrystalline cellulose, croscarm...
Докладніше 127у.е.
In 1 film-coated tablet of 100 mg, it contains: active ingredient: 102.0 mg of canagliflozin hemihydrate...
Докладніше